Amnesia
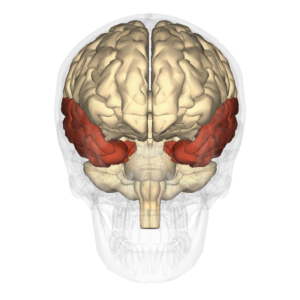
Patients with damage to the temporal lobes may experience anterograde amnesia and/or retrograde amnesia. [Image: en: Anatomography, https://goo.gl/ALPAu6, CC BY-SA 2.1 JP, https://goo.gl/BDF2Z4]
Clearly, remembering everything would be maladaptive, but what would it be like to remember nothing? We will now consider a profound form of forgetting called amnesia that is distinct from more ordinary forms of forgetting. Most of us have had exposure to the concept of amnesia through popular movies and television. Typically, in these fictionalized portrayals of amnesia, a character suffers some type of blow to the head and suddenly has no idea who they are and can no longer recognize their family or remember any events from their past. After some period of time (or another blow to the head), their memories come flooding back to them. Unfortunately, this portrayal of amnesia is not very accurate. What does amnesia typically look like?
The most widely studied amnesic patient was known by his initials H. M. (Scoville & Milner, 1957). As a teenager, H. M. suffered from severe epilepsy, and in 1953, he underwent surgery to have both of his medial temporal lobes removed to relieve his epileptic seizures. The medial temporal lobes encompass the hippocampus and surrounding cortical tissue. Although the surgery was successful in reducing H. M.’s seizures and his general intelligence was preserved, the surgery left H. M. with a profound and permanent memory deficit. From the time of his surgery until his death in 2008, H. M. was unable to learn new information, a memory impairment called anterograde amnesia. H. M. could not remember any event that occurred since his surgery, including highly significant ones, such as the death of his father. He could not remember a conversation he had a few minutes prior or recognize the face of someone who had visited him that same day. He could keep information in his short-term, or working, memory, but when his attention turned to something else, that information was lost for good. It is important to note that H. M.’s memory impairment was restricted to declarative memory, or conscious memory for facts and events. H. M. could learn new motor skills and showed improvement on motor tasks even in the absence of any memory for having performed the task before (Corkin, 2002).
In addition to anterograde amnesia, H. M. also suffered from temporally graded retrograde amnesia. Retrograde amnesia refers to an inability to retrieve old memories that occurred before the onset of amnesia. Extensive retrograde amnesia in the absence of anterograde amnesia is very rare (Kopelman, 2000). More commonly, retrograde amnesia co-occurs with anterograde amnesia and shows a temporal gradient, in which memories closest in time to the onset of amnesia are lost, but more remote memories are retained (Hodges, 1994). In the case of H. M., he could remember events from his childhood, but he could not remember events that occurred a few years before the surgery.
Amnesiac patients with damage to the hippocampus and surrounding medial temporal lobes typically manifest a similar clinical profile as H. M. The degree of anterograde amnesia and retrograde amnesia depend on the extent of the medial temporal lobe damage, with greater damage associated with a more extensive impairment (Reed & Squire, 1998). Anterograde amnesia provides evidence for the role of the hippocampus in the formation of long-lasting declarative memories, as damage to the hippocampus results in an inability to create this type of new memory. Similarly, temporally graded retrograde amnesia can be seen as providing further evidence for the importance of memory consolidation (Squire & Alvarez, 1995). A memory depends on the hippocampus until it is consolidated and transferred into a more durable form that is stored in the cortex. According to this theory, an amnesiac patient like H. M. could remember events from his remote past because those memories were fully consolidated and no longer depended on the hippocampus.
The classic amnesiac syndrome we have considered here is sometimes referred to as organic amnesia, and it is distinct from functional, or dissociative, amnesia. Functional amnesia involves a loss of memory that cannot be attributed to brain injury or any obvious brain disease and is typically classified as a mental disorder rather than a neurological disorder (Kihlstrom, 2005). The clinical profile of dissociative amnesia is very different from that of patients who suffer from amnesia due to brain damage or deterioration. Individuals who experience dissociative amnesia often have a history of trauma. Their amnesia is retrograde, encompassing autobiographical memories from a portion of their past. In an extreme version of this disorder, people enter a dissociative fugue state, in which they lose most or all of their autobiographical memories and their sense of personal identity. They may be found wandering in a new location, unaware of who they are and how they got there. Dissociative amnesia is controversial, as both the causes and existence of it have been called into question. The memory loss associated with dissociative amnesia is much less likely to be permanent than it is in organic amnesia.

