Sexually Transmitted Infections
Unfortunately, a potential outcome of sexual activity is infection. Sexually transmitted infections (STIs) are like other transmittable infections, except STIs are primarily transmitted through social sexual behaviors. Social sexual behaviors include romantic kissing and oral, vaginal, and anal sex. Additionally, STIs can be transmitted through blood, and from mother to child during pregnancy and childbirth. STIs may lead to sexually transmitted diseases (STDs). Often, infections have no symptoms and do not lead to diseases. For example, the most common STI for men and women in the US is Human Papillomavirus (HPV). In most cases, HPV goes away on its own and has no symptoms. Only a fraction of HPV STIs develop into cervical, penile, mouth, or throat cancer (Centers for Disease Control and Prevention, CDCP, December 2016).
There are more than 30 different STIs. STIs differ in their primary methods of transmission, symptoms, treatments, and whether they are caused by viruses or bacteria. Worldwide, some of the most common STIs are: genital herpes (500 million), HPV (290 million), trichomoniasis (143 million), chlamydia (131 million), gonorrhoea (78 million), human immunodeficiency virus (HIV, 36 million), and syphilis (6 million; World Health Organization, 2016).

Sex education is a critical tool in the fight against sexually transmitted infections. [Image: turibamwe, https://goo.gl/ iviJ3U, Public Domain]
Medical testing to determine whether someone has an STI is relatively simple and often free (gettested.cdc.gov). Further, there are vaccines or treatments for all STIs, and many STIs are curable (e.g., chlamydia, gonorrhea, and trichomoniasis). However, without seeking treatment, all STIs have potential negative health effects, including death from some. For example, if untreated, HIV often leads to the STD acquired immune deficiency syndrome (AIDS)—over one million people die every year from AIDs (aids.gov). Unfortunately, many, if not most, people with STIs never get tested or treated. For example, as many as 30% of those with HIV and 90% of those with genital herpes are unaware of having an STI (Fleming et al., 1997; Nguyen & Holodniy, 2008).
It is impossible to contract an STI from a person who does not have an STI. This may seem like an obvious statement, but a recent study asked 596 freshmen- and sophomore-level college students the following True/False question, “A person can get AIDS by having anal (rectal) intercourse even if neither partner is infected with the AIDS virus,” and found that 33% of them answered “true” (Lucas et al., 2016). What is obvious, is that false stereotypes about anal sex causing AIDS continue to misinform our collective sexual knowledge. Only open, honest, and comprehensive education about human sexuality can fight these STI stereotypes. To be clear, anal sex is associated with STIs, but it cannot cause an STI. Specifically, anal sex, when compared to vaginal sex (the second most likely method of transmission), oral sex (third most likely), and romantic kissing (fourth most likely), is associated with the greatest risk of transmitting and contracting STIs, because the tissue lining of the rectum is relatively thin and apt to tear and bleed, thereby passing on the infection (CDCP, 2016).
A sexually active person’s chance of getting an STI depends on a variety of factors. Two of these are age and access to sex education. Young people between the ages of 15 and 24 account for more than 50% of all new STIs, even though they account for only about 25% of the sexually active population (Satterwhite et al., 2013). Generally, young males and females are equally susceptible to getting an STI; however, females are much more likely to suffer long-term health consequences of an STI. For example, each year in the US, undiagnosed STDs cause about 24,000 females to become infertile (CDCP, October 2016; DiClemente, Salazar & Crosby, 2007).
Limited access to comprehensive sex education is also a major contributing factor toward the risk of contracting an STI. Unfortunately, some sex education is limited to the promotion of abstinence, and relies heavily on “virginity pledges.” A virginity pledge is a commitment to refrain from sexual intercourse until heterosexual marriage. Although virginity pledges fit well with some cultural and religious worldviews, they are only effective if people, in fact, remain abstinent. Unfortunately, this is not always the case; research reveals many ways these types of strategies can backfire. Adolescents who take virginity pledges are significantly less likely than other adolescents to use contraception when they do become sexually active (Bearman & Brückner, 2001). Further, virginity pledgers are four to six times more likely than non- pledgers to engage in both oral and anal intercourse (Paik, Sanchagrin & Heimer, 2016), often assuming they’re preserving their virgin status by simply avoiding vaginal sex. In fact, schools with students taking virginity pledges have significantly higher rates of STIs than other schools (Bearman & Brückner, 2001).
Interestingly, senior citizens are one of the fastest growing segments of the European and US populations being diagnosed with STIs. The Centers for Disease Control and Prevention report a steady increase in people over 65 being diagnosed with HIV; since 2007, incidence of syphilis among seniors is up by 52% and chlamydia is up by 32%; and from 2010 to 2014, there was a 38% increase in STI diagnoses in people between the ages of 50 and 70 (Forster, 2016; Weiss, 2014). Why is this happening? Bear in mind, seniors are not necessarily more sexually knowledgeable than adolescents; they may have no greater access to comprehensive sex education than younger people (Adams, Oye & Parker, 2003). Even so, medical advances allow seniors to continue to be sexually active at later points in their lifespan—and to make the same mistakes adolescents make about safer sex.
Safer Sex
STIs are 100% preventable: Simply don’t engage in social sexual behaviors. But in the grand scheme of things, you may be surprised to hear, avoiding sex is detrimental to your physical and mental well-being—whereas, having sex can be widely beneficial (Charnetski & Brennan, 2004; Ditzen, Hoppmann & Klumb, 2008; Hall et al., 2010). Thus, we recommend safer-sex practices, such as communication, honesty, and barrier methods. Safer-sex practices always begin with communication. Before engaging in sexual behaviors with a partner, a clear, honest, and explicit understanding of your boundaries, as well as your partner’s, should be established. Safer sex involves discussing and using barriers—male condoms, female condoms, or dental dams—relative to your specific sexual behaviors. Also, keep in mind: Although safer sex may use some of the same tools as birth control, safer sex is not birth control. Birth control focuses on reproduction; safer sex focuses on well-being.
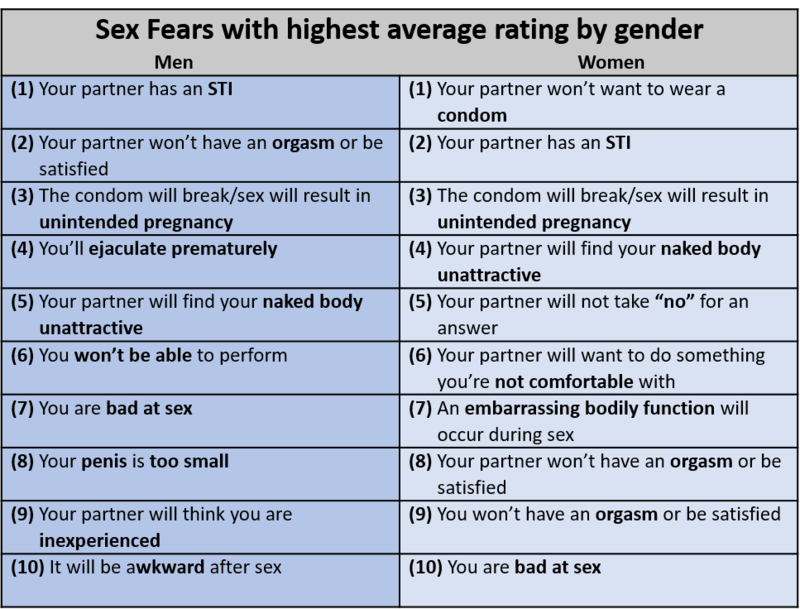
Table 2: Top 10 Fears Men and Women Have During Sex
A proactive approach to behaving sexually may at first seem burdensome, but it can be easily reimagined as “foreplay,” is associated with greater sexual satisfaction, increases the probability of orgasm, and addresses fears people have during sex (see Table 2; Jalili, 2016; Nuno, 2017).

