Physiology and the Sexual Response Cycle
The brain and other sex organs respond to sexual stimuli in a universal fashion known as the sexual response cycle (SRC; Masters & Johnson, 1966). The SRC is composed of four phases:
Excitement: Activation of the sympathetic branch of the autonomic nervous system defines the excitement phase; heart rate and breathing accelerates, along with increased blood flow to the penis, vaginal walls, clitoris, and nipples. Involuntary muscular movements (myotonia), such as facial grimaces, also occur during this phase.
Plateau: Blood flow, heart rate, and breathing intensify during the plateau phase. During this phase, often referred to as “foreplay,” females experience an orgasmic platform—the outer third of the vaginal walls tightening—and males experience a release of pre-seminal fluid containing healthy sperm cells (Killick et al., 2011). This early release of fluid makes penile withdrawal a relatively ineffective form of birth control (Aisch & Marsh, 2014). (Question: What do you call a couple who use the withdrawal method of birth control? Answer: Parents.)
Orgasm: The shortest but most pleasurable phase is the orgasm phase. After reaching its climax, neuromuscular tension is released and the hormone oxytocin floods the bloodstream—facilitating emotional bonding. Although the rhythmic muscular contractions of an orgasm are temporally associated with ejaculation, this association is not necessary because orgasm and ejaculation are two separate physiological processes.
Resolution: The body returns to a pre-aroused state in the resolution phase. Males enter a refractory period of being unresponsive to sexual stimuli. The length of this period depends on age, frequency of recent sexual relations, level of intimacy with a partner, and novelty. Because females do not have a refractory period, they have a greater potential— physiologically—of having multiple orgasms. Ironically, females are also more likely to “fake” having orgasms (Opperman et al., 2014).
Of interest to note, the SRC occurs regardless of the type of sexual behavior—whether the behavior is masturbation; romantic kissing; or oral, vaginal, or anal sex (Masters & Johnson, 1966). Further, a partner or environmental object is sufficient, but not necessary, for the SRC to occur.
Pregnancy
One of the potential outcomes of the SRC is pregnancy—the time a female carries a developing human within her uterus. How does this happen?
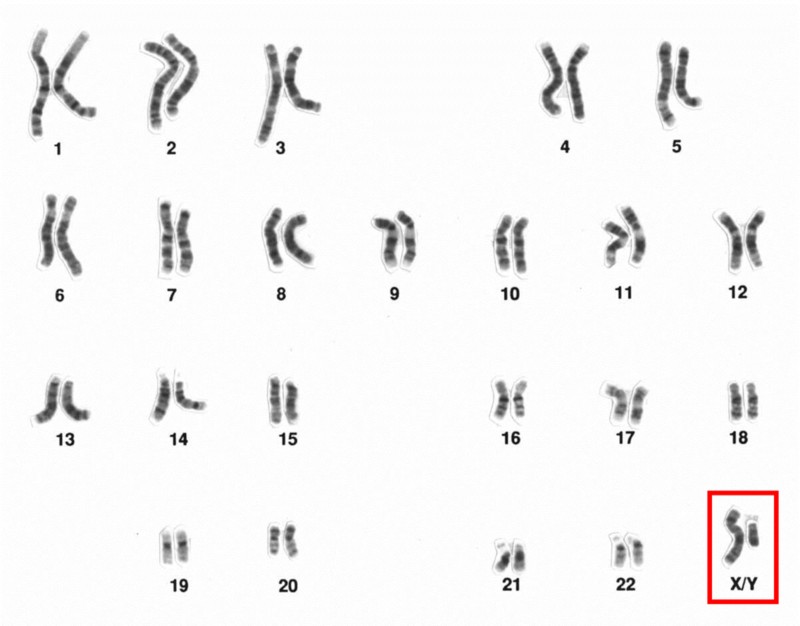
Human male, sex chromosomes highlighted [Image: National Human Genome Research Institute, https://goo.gl/8UWQwa, Public Domain]
The process begins during vaginal intercourse when the male ejaculates, or releases semen. Each ejaculate contains about 300 million sperm cells. These sperm compete to make their way through the cervix and into the uterus. Conception typically occurs within a fallopian tube when a single sperm cell comes into contact with an ovum (egg). The sperm carries either an X- or Y- chromosome to fertilize the ovum— which, itself, usually carries an X- chromosome. These chromosomes, in combination with one another, are what determine a person’s sex. The combination of two X chromosomes produces a female zygote (fertilized ovum). The combination of an X and Y chromosome produces a male zygote. XX- or XY-chromosomes form your 23rd set of chromosomes (most humans have a total of 46 chromosomes) commonly referred to as your chromosomal sex or genetic sex.
Interestingly, at least 1 in every 1,000 conceptions results in a variation of chromosomal sex beyond the typical XX or XY sets. Some of these variations include, XXX, XXY, XYY, or even a single X (Dreger, 1998). In some cases, people may have unusual physical characteristics, such as being taller than average, having a thick neck, or being sterile (unable to reproduce); but in many cases, these individuals have no cognitive, physical, or sexual issues (Wisniewski et al., 2000). Almost 15 out of every 1,000 births are multiple births (twins, triplets, quadruplets, etc.). These can occur in a couple of ways. Dizygotic (fraternal) births are the result of a female releasing multiple ova of which more than one is fertilized by sperm. Because sperm carry either X or Y chromosomes, fraternal births can be any combination of sexes (e.g., two girls or a boy and a girl). They develop together in the uterus and are usually born within minutes of one another. Monozygotic (identical) births result from a special circumstance in which a fertilized ovum splits into multiple identical embryos and they develop simultaneously. Identical twins are, therefore, the same sex.
Hours after conception, the zygote begins dividing into additional cells. It then starts traveling down the fallopian tube until it enters the uterus as a blastocyst. The blastocyst implants itself within the wall of the uterus to become an embryo (Moore, Persaud & Torchia, 2016). However, the percentage of successful implantations remains a mystery. Researchers believe the failure rate to be as high as 60% (Diedrich et al., 2007). Failed blastocysts are eliminated during menstruation, often without the female ever knowing conception occurred.
Mothers are pregnant for three trimesters, a term that begins with their last menstrual period and ends about 40 weeks later; each trimester is 13 weeks. During the first trimester, most of the body parts of the embryo are formed, although at this stage they are not in the same proportions as they will be at birth. The brain and head, for example, account for about half of the body at this point. During the fifth and sixth weeks of gestation, the primitive gonads are formed. They eventually develop into ovaries or testes. Until the seventh week, the developing embryo has the potential of having either male (Wolffian ducts) or female (Mullerian ducts) internal sex organs, regardless of chromosomal sex. In fact, there is an innate tendency for all embryos to have female internal sex organs, unless there is the presence of the SRY gene, located on the Y-chromosome (Grumbach & Conte, 1998; Wizemann & Pardue, 2001). The SRY gene causes XY-embryos to develop testes (dividing cells from the medulla). The testes emit testosterone which stimulates the development of male internal sex organs—the Wolffian ducts transforming into the epididymis, seminal vesicles, and vas deferens. The testes also emit a Mullerian inhibiting substance, a hormone that causes the Mullerian ducts to atrophy. If the SRY gene is not present or active—typical for chromosomal females (XX)—then XX-embryos develop ovaries (dividing cells from the cortex) and the Mullerian ducts transform into female internal sex organs, including the fallopian tubes, uterus, cervix, and inner two-thirds of the vagina (Carlson, 1986). Without a burst of testosterone from the testes, the Wolffian ducts naturally deteriorate (Grumbach & Conte, 1998; Wizemann & Pardue, 2001).
During the second trimester, expectant mothers can feel movement in their wombs. This is known as quickening. Inside the uterus, the embryo develops fine hair all over its body (called lanugo) as well as eyelashes and eyebrows. Major organs, such as the pancreas and liver, begin fully functioning. By the 20th week of gestation, the external sex organs are fully formed, which is why “sex determination” using ultrasound during this time is more accurate than in the first trimester (Igbinedion & Akhigbe, 2012; Odeh, Ophir & Bornstein, 2008). Formation of male external sex organs (e.g., the penis and scrotum) is dependent upon high levels of testosterone, whereas female external sex organs (e.g., the outer third of the vagina and the clitoris) form without hormonal influences (Carlson, 1986). Levels of sex hormones, such as estrogen, testosterone, and progesterone, begin affecting the brain during this trimester, impacting future emotions, behaviors, and thoughts related to gender identity and sexual orientation (Swaab, 2004). It’s important to understand that the interactions of chromosomal sex, gonadal sex, sex hormones, internal sex organs, external sex organs, and brain differentiations during this developmental stage are too complex to readily conform to the familiar categories of sex, gender, and sexual orientation historically used to describe people (Herdt, 1996). Toward the end of the second trimester—at about the 26th week—is the age of viability, when survival outside of the uterus has a probability of more than 90% (Rysavy et al., 2015). Interestingly, technological advances and changes in hospital care have affected the age of viability such that viability is possible earlier in pregnancy (Rysavy et al., 2015).
During the third trimester, there is rapid development in the brain and rapid weight gain. Typically, by the 36th week, the fetus begins descending head-first into the uterine cavity. Getting ready for birth is not the only behavior exhibited during this last trimester. Erectile responses in male fetuses occur during this time (Haffner, 1999; Martinson, 1994; Parrot, 1994); and Giorgi and Siccardi (1996) reported ultrasonographic observations of a fetus performing self-exploration of her external sex organs. Most babies are born vaginally (through the vagina), though in the United States one-third are by Cesarean section (through the abdomen; Molina et al., 2015). A newborn’s health is initially determined by his/her weight (normally ranging between 2,500 and 4,000 grams)—though birth weight significantly differs between ethnicities ( Jannsen et al., 2007).

Potential outcomes of the Sexual Response Cycle are pregnancy and childbirth. [Image: Ernest F, https://goo.gl/TPu7g8, CC BY- SA 3.0, https://goo.gl/jidmcs]
Birth Control
Contraception, or birth control, reduces the probability of pregnancy resulting from sexual intercourse. There are various forms of birth control, including: hormonal, barrier, or natural. As shown in Table 1, the effectiveness of the different forms of birth control ranges widely, from 68% to 99.9% (optionsforsexualhealth.org).
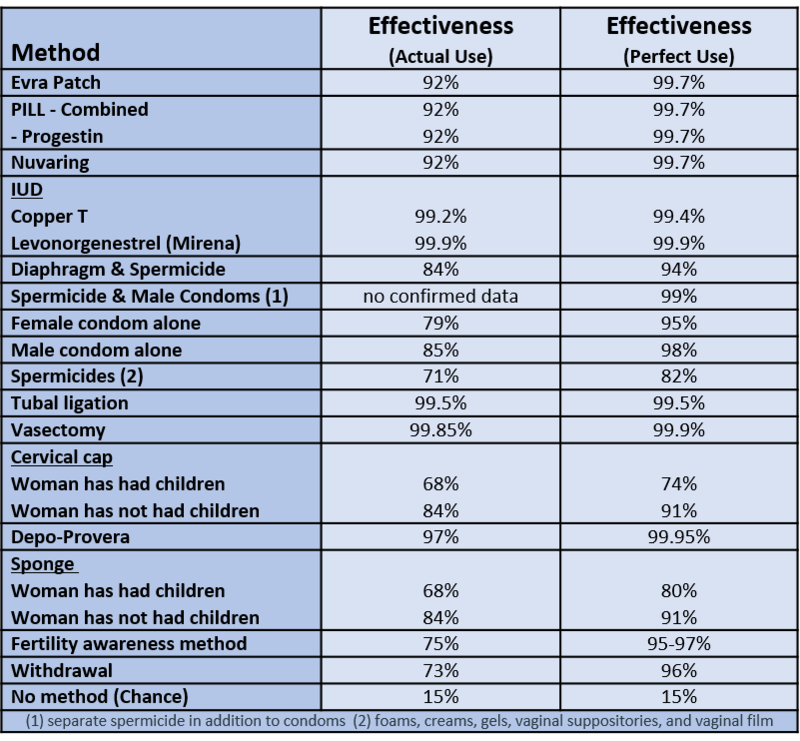
Table 1. Forms of Birth Control and their Effectiveness – from https://www.optionsforsexualhealth.org/
Hormonal forms of birth control release synthetic estrogen or progestin, which prevents ovulation and thickens cervical mucus, making it difficult for sperm to reach ova (sexandu.ca/contraception). There are a variety of ways to introduce these hormones into the body, including: implantable rods, birth control pills, injections, transdermal patches, IUDs, and vaginal rings. For example, the vaginal ring is 92% effective, easily inserted into and taken out of the vagina by the user, and comprised of thin plastic containing a combination of hormones that are released during the time it is in the vagina—usually about three weeks.
Barrier forms of birth control prevent sperm from entering the uterus by creating a physical barrier or chemical barrier toxic to sperm. There are a variety of barrier methods, including:
vasectomies, tubal ligations, male and female condoms, spermicides, diaphragms, and cervical caps. The most popular barrier method is the condom, which is 79-85% effective. The male condom is placed over the penis, whereas the female condom is worn inside the vagina and fits around the cervix. Condoms prevent bodily fluids from being exchanged and reduce skin-to-skin contact. For this reason, condoms are also used to reduce the risk of some sexually transmitted infections (STIs). However, it is important to note that male and female condoms, or two male condoms, should not be worn simultaneously during penetration; the friction between multiple condoms creates microscopic tears, rendering them ineffective (Munoz, Davtyan & Brown, 2014).
Natural forms of birth control rely on knowledge of the menstrual cycle and awareness of the body. They include the Fertility Awareness Method (FAM), lactational amenorrhea method, and withdrawal. For example, the FAM is about 75% effective, and requires tracking the menstrual cycle, and avoiding sexual intercourse or using other forms of birth control during the female’s fertile window. About 30% of females’ fertile windows—the period when a female is most likely to conceive—are between days ten and seventeen of their menstrual cycle (Wilcox, Dunson & Baird, 2000). The remaining 70% of females experience irregular and less predictable fertile windows, reducing the efficacy of the FAM.
Other forms of birth control that do not fit into the above categories include: emergency contraceptive pills, the copper IUD, and abstinence. Emergency contraceptive pills (e.g., Plan B) delay the release of an ovum if taken prior to ovulation. Emergency contraception is a form of birth control typically used after unprotected sex, condom mishaps, or sexual assault. The most effective form of emergency contraception is the copper IUD. A medical professional inserts the IUD through the opening of the cervix and into the uterus. It is more than 99% effective and may be left within the uterus for over 10 years. It differs from typical IUDs because it is hormone-free and uses copper ions to create an inhospitable environment for sperm, thus significantly reducing the chances of fertilization. Additionally, the copper ions alter the lining of the uterus, which significantly reduces the probability of implantation. Lastly, abstinence—avoiding any sexual behaviors that may lead to conception—is the only form of birth control with a 100% effective rate.
There are many factors that determine the best birth control options for any particular person. Some factors are related to personality and habits. For example, if a woman is a forgetful person, “the pill” may not be her best option, since it requires being taken daily. Other factors that influence birth control choices include cost, age, education, religious beliefs, lifestyle, and sexual health.

