Part 3: Sustainability Issues in Planetary Health
12 Sustainable Healthcare Delivery
Learning Objectives
After reading this chapter the learner should be able to:
- Define sustainable healthcare delivery
- Identify current leaders and initiatives in sustainable healthcare
- Define co-benefits and describe how co-benefits relate to health
- Define the built environment and identify the role of different disciplines within the built environment
Keywords
Essential Key words for this chapter include:
- sustainability
- sustainable healthcare
- healthcare delivery
- health outcomes
- conscientious healthcare
- green healthcare
- built environment
- interdisciplinary collaboration
Section 1: The importance of practicing sustainable healthcare delivery
Background
In 2015, pollution was estimated to be responsible for 9 million premature deaths; which comprised 16% of global deaths (Landrigan et al., 2018). According to the Lancet Commission on Pollution and Health report (2018):
Exposures to contaminated air, water, and soil kill more people than a high-sodium diet, obesity, alcohol, road accidents, or child and maternal malnutrition. They are also responsible for three times as many deaths as AIDS, tuberculosis, and malaria combined, and for nearly 15 times as many deaths as war and all forms of violence. (Landrigan, et al., 2018, p. 1).
Many of the pollutants that harm our health are major greenhouse gasses (GHGs) and are harming the health of our planet’s natural systems (Landrigan, et al., 2018). Human sectors contribute to the emission of these pollutants and GHGs, with healthcare being a top emitter. In fact, it has been suggested that if the global health sector were considered a country and its emissions were compared to that of other countries, it would be the fifth-largest emitter in the world,responsible for approximately 4.4% of global net emissions (Healthcare Without Harm [HCWH] & Arup, 2019). Besides harming our natural systems and being a significant contributor to climate change, these GHGs and pollutants are linked with negative human health outcomes. In Canada it is estimated that healthcare’s emissions alone result in 23, 000 disability-adjusted life years lost annually (Eckelman et al., 2018).
Interestingly, when ranked against other national healthcare systems, Canada’s health sector is considered the 9th worst GHG emitter. However, if you look at emissions on a per capita basis, one begins to see a different picture; Canada’s health sector is the second highest GHG emitting healthcare system on a per capita basis. In other words, while in total our health system does not emit as much as other health systems do globally, when emissions are examined on a per capita basis (i.e., on the basis of how many emissions are produced on the basis of each individual healthcare user), Canadians are emitting significantly more GHGs (over 1 metric ton of carbon dioxide emitted per person) than citizens of other countries. This indicates that the Canadian health sector still has a great deal of work to do in terms of developing a healthcare system that is sustainable and promotes the health of our natural systems and humanity.
Generally speaking, the health sector’s main purpose around the world is to protect and promote human health, but due to its significant emissions, it can be paradoxically stated that the health sector, directly and indirectly, harms human health. Moreover, the health sector’s organizational systems and structures are extremely vulnerable to the effects of climate change (Smith et al., 2014). Considering healthcare’s climate vulnerability and its moral and ethical mandate to support, protect, and maintain human health, it is clear that now, more than ever, there is a critical need for a healthcare system that is sustainable and driven by a planetary health perspective.
Healthcare professionals (doctors, nurses, midwives, and others) are essential players in the development of sustainable healthcare systems as they are uniquely situated to be leaders in this field. These professionals both act on what science and research demonstrate as best evidence and speak with ethical and moral authority. Healthcare professionals are often the most trusted professionals in the eyes of the public and can help persuade people and nations to reduce their emissions and strive for a healthy planet. “Most importantly, they are powerful advocates for the very thing that people worldwide care about most and are most threatened by climate change: our health and well-being and that of future generations” (Al-Delaimy, Ramanathan, and Sanchez Sorondo, 2020, p. 396).
Healthcare Emissions
Generally speaking, every country’s health system directly and indirectly emits GHGs via product procurement, active care delivery, and services and technologies from a carbon-intensive supply chain (HCWH & Arup, 2019). The most significant source of emissions (71%) are derived from healthcare’s supply chain via production, transportation, and disposal of goods and services such as pharmaceuticals, food and agricultural products, medical devices, hospital equipment, and instruments. (HCWH & Arup, 2019). Another 17% of emissions result directly from healthcare facilities and vehicles owned by health organizations. The final 12% are indirect emissions that are derived from purchased energy, such as electricity, steam, cooling, and heating (HCWH & Arup, 2019). “Fossil fuel consumption is at the heart of health care’s emissions. Energy — primarily the combustion of fossil fuels — makes up well over half of health care’s climate footprint when measured across all three scopes” (HCWH & Arup, 2019, p. 4).
Theoretical Models
We can use theory to help guide our thinking regarding the problems and solutions related to the development of sustainable healthcare systems. Theory gives us a unified starting point when examining sustainable healthcare systems. We propose Systems Thinking Theory as one that is useful for our explorations.
Systems Thinking Theory
Traditional healthcare systems and education have been built on mechanistic, cause-and-effect scientific models. While historically helpful, these models are limited in that they “do not fully explain the complexity of humans, our relationships and the interconnectedness of all life” (Al-Delaimy, Ramanathan and Sanchez Sorondo, 2020, p. 213). If we are going to succeed in promoting planetary health and limiting the pressure humanity is placing on our planetary boundaries (Image 1), a more holistic model of health is necessary. Planetary boundaries refer to the limits placed on our planet via anthropogenic forces (i.e., climate change, freshwater usage, land-system changes, etc.); there are safe operating zones, zones of uncertainty, and beyond the zones of uncertainty which identify high risk to planetary health (Steffen et al., 2015). A holistic model of healthcare suggests that we are dynamic, social, and complex beings that are in constant, intimate relationships with all other living things on Earth. “Individual, community, and planetary health are inseparable” (Al-Delaimy, Ramanathan and Sanchez Sorondo, 2020, p. 213). This holistic perspective is at the heart of planetary health and is necessary for the development of sustainable healthcare; we require a health system that promotes both human health as well as the health of our planet and its natural systems.
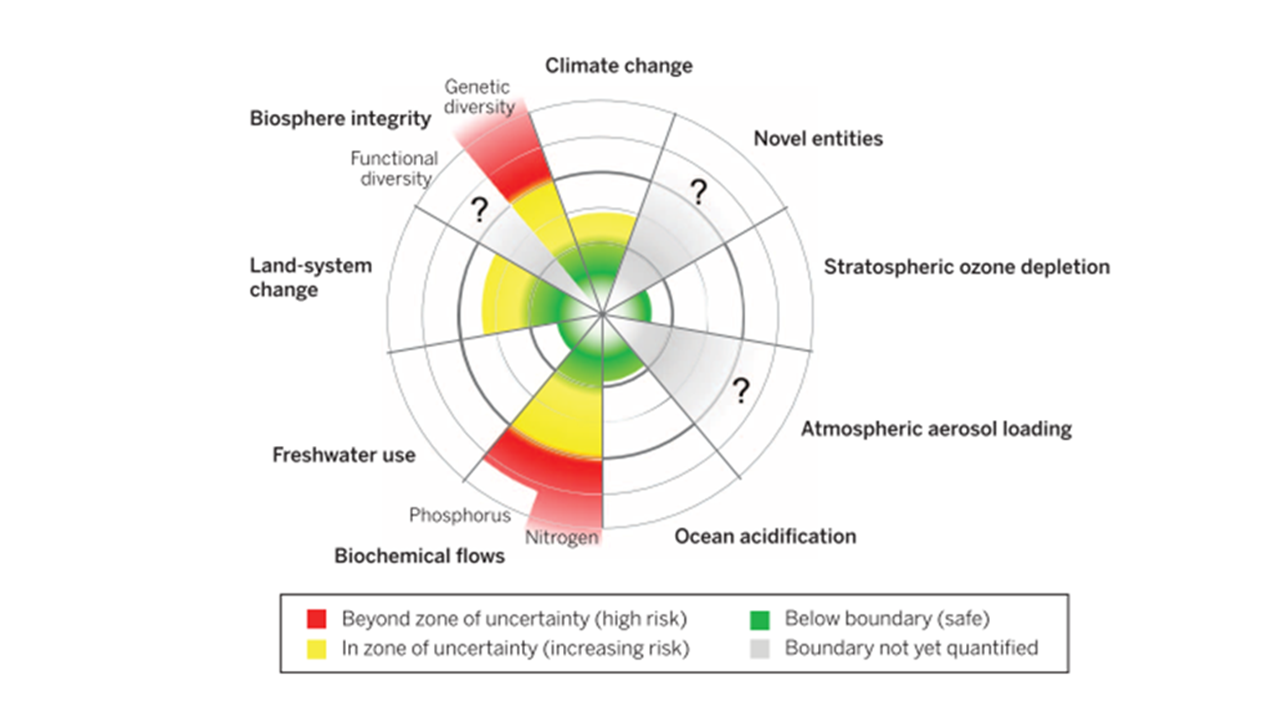
Image 1: Planetary boundaries (Steffen et al., 2015)
What is Sustainable Healthcare?
Sustainability is a complex term with consistent themes in the literature, such as the idea that we need to work on things now so that we (and future generations) can enjoy them in the future (Schroeder et al., 2013). Sustainability is concerned with relationships and the interconnectedness of our planet and its natural system; it is concerned with resource preservation, reducing our consumption, and appropriate disposal of waste products. When we think sustainably, we acknowledge the planetary boundaries and look for ways to thrive while remaining safely within them; we view humanity as guardians of the planet’s natural systems and resources, not as its owners. Finally, there is a distinct leaning towards upholding social justice. In other words, sustainability inherently recognizes that it is unjust for some communities to exploit the earth’s natural resources at the expense of others.
Thus, sustainable healthcare refers to the delivery of healthcare services that does not put detrimental stress on either human or natural systems (Schroeder et al., 2013). It is a style of healthcare delivery that consciously works at promoting planetary health by reducing its GHG emissions, waste, and overall environmental impact. Health systems can achieve this through various methods, and some examples include retrofitting buildings so that they run on more sustainable sources of energy, offering more plant-based meals for patients and their families as it is known that meat and associated farming practices are extremely carbon intensive, reducing consumption of resources and materials and properly diverting waste, paying attention to transportation GHGs associated with either health system processes (e.x., driving lab samples to a local laboratory for analysis) or with traveling to/from the health building (e.x., patients traveling to the hospital to access medical services or healthcare employees getting to work), and addressing and decarbonizing the supply chains associated with procuring healthcare equipment and resources. This is not an exhaustive list, and there are many ways to reduce healthcare’s planetary impact when paying attention to these areas and beyond. In fact, several leaders are already starting to do this important work.
Organizational Leaders in Sustainable Healthcare
Many leaders worldwide are already contributing to sustainable healthcare systems, such as the Canadian Coalition for Green Health Care (CCGH) and Health Care Without Harm (HCWH). The CCGH is a national group that works closely with individuals, agencies/organizations, and others who are actively involved in healthcare delivery by sharing best practices related to sustainable healthcare delivery. HCWH works with healthcare delivery leaders and supports them in several areas: Canadian health sector data collection, green leadership, green purchasing, health and environment, local and sustainable Foods, safer chemical policies/toxics reduction, sustainable buildings, sustainable energy and GHG, sustainable transportation, and finally, waste management and minimization (Canadian Coalition for Green Health Care, n.d.).
HCWH’s main mission is to transform healthcare worldwide so that the sector can be a world leader in the global movement for health and justice (Health Care Without Harm, n.d.). More concretely, they have actively made international healthcare systems more sustainable through various initiatives, including (but not limited to): a) helping close more than 4,400 incinerators that burned carcinogenic medical waste (which helped hospitals save money, reuse and reprocess resources, and utilize alternative waste treatment strategies); b) they launched the Health Care Climate Challenge – an initiative that has over 300 participating institutions (representing over 22,000 hospitals) across 40 countries committing to climate action; c) created the Greenhealth Approved program which helps healthcare providers quickly identify safe, sustainable products and thereby supporting them in making the often challenging decisions of whether a product is more/less harmful for the environment; and d) supported hundreds of hospitals in adopting the “green operating room” strategy, which helps save money and valuable resources while also reducing pollution and waste (Health Care Without Harm, n.d.).
Role of Healthcare Professionals
Healthcare professionals play a key role in developing sustainable health systems. First, they must educate the public, developers, and decision makers about the health consequences of ignoring planetary health. Second, health professionals should conduct research that explores and expands the intersection between planetary health, climate change, climate action, and healthcare. This research must be translated into easy-to-read/understand material for the public so they can also incorporate this information into their daily lives (Kalogirou et al., 2020; Landrigan et al., 2018). Finally, and perhaps most importantly, health professionals must advocate for planetary health.
Research suggests that advocacy requires both a top-down and a bottom-up approach (Kalogirou et al., 2021). In other words, while significant change is required to come from decision-makers and leaders in the health sector (top-down), health professionals and even healthcare users need to advocate for the prioritization of planetary health and push leadership in this direction (bottom-up). Without this bottom-up advocacy and a clear demonstration from health professionals that planetary health is important to strive for, it is unlikely that decision-makers will make the necessary changes quickly. One clear way for healthcare professionals to advocate for the integration and prioritization of planetary health is to “reclaim [their roles] at the heart of environment and development policies, taking a more proactive approach.” (Al-Delaimy, Ramanathan and Sanchez Sorondo, 2020, p. 97). For example, nurses in one study objected to the practice of disposing narcotics down the drain; they recognized that the narcotics were getting into water systems and harming surrounding natural systems (King and McCue, 2017). The nurses advocated for a change in policy and a change in what it meant to properly dispose of narcotics in their workplace. Another example includes doctors who objected to the use of certain anesthetic gasses in the operating room on the premise of them being harmful GHGs. These doctors also advocated for changes in policy and practice to support the health of people and our planet (Özelsel, Sondekoppam & Buro, 2019).
Outcomes of Sustainable Healthcare
The outcomes of sustainable healthcare may be best explored through the lens of co-benefits. According to Schroeder et al. (2017), co-benefits have a triple bottom-line: healthy planet, healthy people, and economic profit. In other words, co-benefits are actions that are good for the planet and for either human health or the economy. An example of a co-benefit is related to Canada’s plans to phase out coal-fired power by 2030; this will avoid more than 1,000 premature deaths associated with corresponding air pollution and yield an additional $5 billion in health benefits by 2035 (Environment and Climate Change Canada, 2021). Another example can be seen through the image below (Image 2). Health, wellbeing, equity, and environmental concerns are all addressed when societies consider urban planning and power generation and provide equitable access to clean household energy and low-carbon electricity. By addressing key indicators related to climate mitigation (urban planning, power generation, transportation, industry, healthcare, and agriculture and forestry), we can improve the health and wellbeing of populations. The role of the healthcare professional is to consider the stance of co-benefits, and then advocate and lobby governments and organizations to prioritize the actions necessary to promote planetary health.
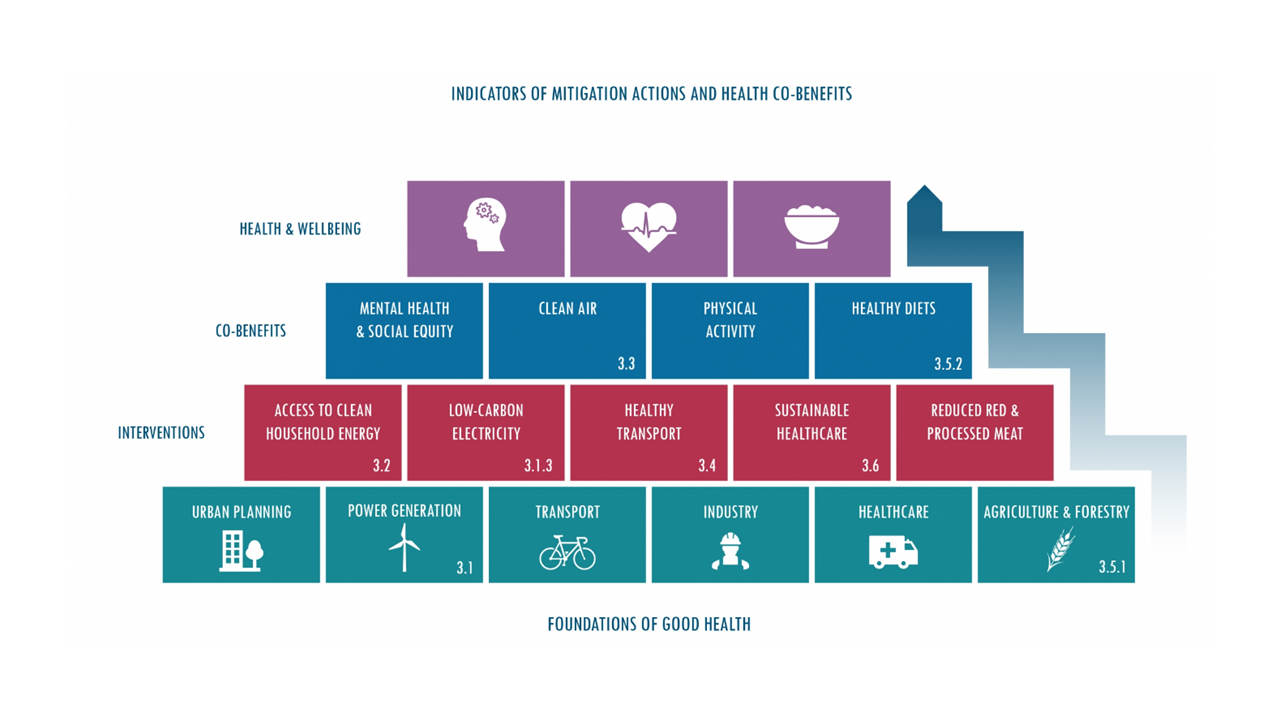
Figure 2. Foundations of Good Health
Table 1: Practical Actions for Healthcare Practitioners and Green Teams
| PROBLEM | HEALTHCARE PROFESSIONAL ACTIONS | OUTCOME |
|---|---|---|
| Levels of GHGs associated with food production are immense. Animal farming is extremely resource-intensive and food waste is a significant source of emissions. Moreover, “[the] global economic, environmental, and social cost of food wastage is estimated at US$2.6 trillion” (Project Drawdown, n.d.). | 1. Working with food services to offer more plant-based food options that are locally sourced.
2. Reducing food waste via appropriate portion sizes and composting food scraps. |
1. If 50–75% of people adopt a healthy diet of about 2,300 calories per day and reduce meat consumption overall, around 54.19–78.48 gigatons of GHGs could be avoided at minimum (Hawken, 2017).
2. Reducing food waste can result in the reduction of 88.50–102.20 gigatons of GHGs (Hawken, 2017). |
| Production of new materials is a significant contributor to GHG emissions. As our consumption of resources continues to increase, so does the environmental footprint of extraction of raw materials (Hawken, 2017). | Analyzing waste management practices, assessing what waste can be reduced, reused, recycled, and what alternatives exist to incineration. | About 50% of recycled materials come from households, while the rest from industry. If the average worldwide recycling rate of metals, plastic, glass, and other materials, such as rubber, textiles, and e-waste increased to 62–82% of total recyclable municipal solid waste, recycling could avoid 10.36–11.29 gigatons of carbon dioxide equivalent emissions by 2050 (Hawken, 2017). |
| In 2018, humanity walked an average of 200 kilometers per person per year. This equates to less than seven minutes of walking per day. We drive seven times as much as we walk. The International Energy Agency estimated that the transportation sector produced 9.5 gigatons of carbon dioxide equivalent emissions in 2018 (International Energy Agency, 2018). | Assessing transportation associated with: a) the organization. Finding local suppliers whenever possible and streamlining transportation routes; b) staff and patients. Organizing and incentivising alternative low-carbon options such as ride-shares, walking groups, or biking competitions. |
1. If public transit is used for 29-34% of all urban passenger trips, this could save 9.42–15.42 gigatons of GHG emissions from cars.
2. Carpooling has no implementation costs. It can reduce emissions by 9.6-11.07 gigatons of carbon dioxide while saving approximately US$7.40–9.18 trillion. 3. It is assumed that an increase in bicycle infrastructure will drive bicycling from under 3% to almost 5–6% of urban trips globally by 2050. This would avoid 2.73–4.63 gigatons of carbon dioxide equivalent emissions. |
(Kalogirou et al., 2020; Kurth, 2017; Sayre et al., 2010)
Health Professionals and the Built Environment
The environment is more than an area’s trees, cars, people, and wildlife. It represents the totality of life and various interactions among and between people and any area of the planet. The built environment consists of many features that have been constructed and modified by humanity. For example, how rooms are laid out, the construction of homes and various land uses in a neighborhood. The built environment even extends to the structure of neighborhoods in metropolitan areas, to the way regional and national geography and infrastructure interact to protect from natural disasters.
The built environment provides a blueprint for how our daily lives are conducted, it influences health across life spans (both human and animal), and represents important pathways through which individuals come into contact with many health risks. There is growing evidence that some environments promote health, while others increase morbidity and mortality. However, the associations between the built environment and health have only been examined closer over the past two decades, and efforts to implement interventions to address health concerns pertaining to the built environment are only in their infancy (Elf, Anåker, Marcheschi, Sigurjónsson, & Ulrich, 2020; Lopez, 2012).
Features of the built environment reflect the interplay of economic, political, and other similar factors. Some of these factors directly influence the built environment; others are more indirect. These include, but are not limited to:
- Laws: development takes place within a legal and constitutional framework
- Geology: soils, coastlines, tectonic factors
- Economics: economic trends, incomes, local economic factors
- Personal and societal values: neighborhood preferences, social factors
- Health assumptions: beliefs regarding causes of morbidity and mortality
- Ideology and political theory: theories of poverty, personal liberty, private property
- Technology: automobiles, Internet, pollution prevention
- Science: research, theories
Collaboration between interdisciplinary professionals (i.e., healthcare providers, welfare, social work) are becoming key elements to support the built environment through efficient and productive efforts at promoting health. Interprofessional teams have been found to increase provider and patient satisfaction, reduce the number of medical errors and other patient safety issues, promote workforce retention and reduce system inefficiencies resulting in higher costs. (Al-Delaimy, Ramanathan and Sanchez Sorondo, 2020; Lopez, 2012). The table below summarizes different professional groups that contribute to the built environment, and their roles.
Table 2. Healthcare Without Harm
| Area of Interest | Description |
|---|---|
| Public Health | Closely related to but broader than medicine, public health is concerned with the health of groups as well as individuals; practitioners focus more on prevention of disease and preservation of health than they do on diagnosis and treatment of individual illnesses. Public health professionals conduct studies, design interventions, administer programs, and evaluate services. |
| Architecture | Architectural practice can range from the design of open spaces (usually referred to as landscape architecture) to the design of individual buildings, neighborhoods, or cities. As will be seen, architecture is heavily influenced by theories of design and has a long history of trying to improve health. However, it should be noted that architects are not the only designers of buildings. Many are designed by engineers, and the design of buildings in developed societies is heavily shaped by building and other safety codes. |
| Ecology | Ecological analysis and environmental science have played an important role in shaping the built environment. Through its tools that include the concept of an ecosystem being a series of energy flows, for example, it assists in the understanding of how the built environment can shape human behavior. |
| Economics | There are many subfields within economics and though some may seem far removed from the study of the built environment, even the most distant can provide insight on the impacts of the built environment. For example, macro economics, which includes the size and rate of expansion of the money supply, can have an impact on the built environment through interest rates, which can either promote speculative building or severely curtail construction activity. |
| Epidemiology | This subfield of public health focuses on the factors that cause, prevent, and may influence disease. Epidemiology is a technical field that uses a number of statistical and other techniques that aim to provide basic scientific evidence that may inform health practice and public policy. |
| Landscape Architecture | Landscape architects tend to design the outdoor spaces for a given project or for a larger community. They may often work closely with architects and urban designers in these efforts. |
| Law | The legal framework of a society profoundly impacts what can be built where. Therefore the study of the law, the identification of how laws are made and how they have been implemented, can assist in our understanding of how the built environment is constructed or how it can be improved. |
| Medicine | Physicians are on the front line of diagnosing and treating disease. Though many doctors also have public health degrees and work extensively in public health, most physicians’ preventive health services are performed on the individual rather than the population level. |
| Nursing | Nurses work with physicians and others to provide direct care to patients. Many nurses also work on the population level to help address health risk behaviors and other types of preventative interventions. |
| Sanitary Science | Taking their name from the great sanitary surveys of the nineteenth century, sanitarians are those professionals involved in implementing laws and regulations meant to protect public health, including food safety, water quality, and other similar types of inspections and enforcement. |
| Sociology | Sociologists, along with their colleagues, anthropologists, study the rich texture of human interactions and how individuals see themselves in relationship to others. They also study human behaviors and the behaviors of groups. |
| Urban Design | An urban designer often works on the overall physical appearance of, and relationships between, buildings, streets, and open spaces over an area that can range from an individual parcel to an entire community. In contrast to urban planners, who tend to focus on programs and policies, urban designers usually produce plans and design guidelines targeted to a specific location. |
| Urban Planning | This field aims to shape and influence the overall nature of neighborhoods, cities, and metropolitan areas. Many urban planners focus on designing and implementing policies and programs that promote economic development, create affordable housing, provide emergency services, administer public programs, manage infrastructure, plan transportation improvements, and so on. |
(Lopez, 2012)
References
Al-Delaimy, W., Ramanathan, V., & Sánchez Sorondo, M. (2020). Health of People, Health of Planet and Our Responsibility. [electronic resource] : Climate Change, Air Pollution and Health (1st ed. 2020.). Springer International Publishing.
Canadian Coalition for Green Health Care, (n.d.). Who We Are. The Canadian Coalition for Green Health Care. Retrieved July 20, 2022, from https://greenhealthcare.ca/who-we-are/
Eckelman, M. J., Sherman, J. D., & Macneill, A. J.. (2018). Life cycle environmental emissions and health damages from the Canadian healthcare system: An economic-environmental-epidemiological analysis. PLOS Medicine, 15(7), e1002623. https://doi.org/10.1371/journal.pmed.1002623
Elf, M., Anåker, A., Marcheschi, E., Sigurjónsson, Á., Ulrich, R.S., 2020. The built environment and its impact on health outcomes and experiences of patients, significant others and staff—A protocol for a systematic review. Nursing Open 7, 895–899.. doi:10.1002/nop2.452
Environment and Climate Change Canada (2021). Canada’s Climate Actions for a Health Environment and a Health Economy. Government of Canada. Retrieved July 20, 2022, from https://www.canada.ca/en/services/environment/weather/climatechange/climate-plan/climate-plan-overview/actions-healthy-environment-economy.html
Hawken, P. (Ed.). (2017). Drawdown: The most comprehensive plan ever proposed to reverse global warming. Penguin Books.
Health Care Without Harm, (n.d.). About Us. Health Care Without Harm. Retrieved July 20, 2022, from https://greenhealthcare.ca/who-we-are/
Health Care Without Harm [HCWH] & Arup. (2019). Health care’s climate footprint: How the health sector contributes. Retrieved from https://noharm-uscanada.org/ClimateFootprintReport
International Energy Agency. (2016). Energy Technology Perspectives 2016: Towards Sustainable Urban Energy Systems. OECD International Energy Agency. https://iea.blob.core.windows.net/assets/37fe1db9-5943-4288-82bf-13a0a0d74568/Energy_Technology_Perspectives_2016.pdf
Kalogirou, M. R., Dahlke, S., Davidson, S., & Yamamoto, S. (2020). Nurses’ perspectives on climate change, health, and nursing practice. Journal of Clinical Nursing, 29(23-24), 4759-68. https://doi.org/10.1111/jocn.15519
Kalogirou, M. R., Dahlke, S., Davidson, S., & Yamamoto, S., (2021). How the hospital setting influences environmentally responsible practice: A focused ethnography. Journal of Advanced Nursing, 77(9), 3806-19. doi:10.1111/jan.14936
King, C., & McCue, A. (2017). Drugs down the drain: When nurses object. Nursing Ethics, 24(4), 452– 461. https://doi.org/10.1177/09697 33015 614882
Kurth, A. E. (2017). Planetary health and the role of nursing: A call to action. Journal of Nursing Scholarship, 49(6), 598-605. https://doi. org/10.1111/jnu.12343
Schroeder, K., Thompson, T., Frith, K., & Pencheon, D. (2013). Sustainable healthcare. BMJ Books
Landrigan, P. J., Fuller, R., Acosta, N. J. R., Adeyi, O., Arnold, R., Basu, N. (Nil) ., Baldé, A. B., Bertollini, R., Bose-O’Reilly, S., Boufford, J. I., Breysse, P. N., Chiles, T., Mahidol, C., Coll-Seck, A. M., Cropper, M. L., Fobil, J., Fuster, V., Greenstone, M., Haines, A., … Zhong, M.. (2018). The Lancet Commission on pollution and health. The Lancet, 391(10119), 462–512. https://doi.org/10.1016/s0140-6736(17)32345-0
Lopez, R. P. (2012). The built environment and public health. John Wiley & Sons, Incorporated.
Markandya, A., Sampedro, J., Smith, S. J., Van Dingenen, R., Pizarro-Irizar, C., Arto, I., & González-Eguino, M.. (2018). Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. The Lancet Planetary Health, 2(3), e126–e133. https://doi.org/10.1016/s2542-5196(18)30029-9
Özelsel, T. J.-P., Sondekoppam, R. V., & Buro, K. (2019). The future is now—it’s time to rethink the application of the Global Warming Potential to anesthesia. Canadian Journal of Anesthesia/journal Canadien D’anesthésie, 66(11), 1291–1295. https://doi.org/10.1007/s12630-019-01385-w
Project Drawdown. (n.d.). Reduced food waste. Retrieved August 4, 2022, from https://www.drawdown.org/solutions/reduced-food-waste
Sayre, L., Rhazi, N., Carpenter, H., & Hughes, N. L. (2010). Climate change and human health: The role of nurses in confronting the issue. Nursing Administration Quarterly, 34(4), 334-342. https://doi. org/10.1097/NAQ.0b013 e3181 f60df9
Smith, K. R., Woodward, A., Campbell- Lendrum, D., Chadee, D. D., Honda, Y., Liu, Q., Olwoch, J. M., Revich, B., & Sauerborn, R. (2014). Human health: Impacts, adaptation, and co- benefits. In C. B. Field, V. R. Barros, D. J. Dokken, K. J. Mach, M. D. Mastrandrea, T. E. Bilir, M. Chatterjee, K. L. Ebi, Y. O. Estrada, R. C. Genova, B. Girma, E. S. Kissel, A. N. Levy, S. MacCracken, P. R. Mastrandrea, & L. L. White (Eds.), Climate change 2014: Impacts, adaptation, and vulnerability. Part A: Global and sectoral aspects (pp. 709– 754). Intergovernmental Panel on Climate Change.
Steffen, W., Richardson, K., Rockström, J., Cornell, S. E., Fetzer, I., Bennett, E. M., Biggs, R., Carpenter, S. R., De Vries, W., De Wit, C. A., Folke, C., Gerten, D., Heinke, J., Mace, G. M., Persson, L. M., Ramanathan, V., Reyers, B., & Sörlin, S. (2015). Planetary boundaries: Guiding human development on a changing planet. Science, 347(6223). https://doi.org/10.1126/science.1259855

