Part 4: Planetary Health Impact on Humans
14 Planetary Health and Infectious Diseases
Authors: Tabarsi, N., & Grynszpan, D.
What’s in this chapter?
- What are Emerging Infectious Diseases (EIDs)?
- What is zoonosis?
- What are the epidemiological considerations?
- What is the relationship to human health? (acute and chronic)
- Physical, mental, and social implications
Learner Outcomes
After reading this chapter you should be able to:
- List key modalities in which the ecosystem and human infectious diseases are interconnected
- Describe the impact that changes in the climate and the ecosystem can have on human infectious diseases
- Explain the emergence of novel human infectious diseases from zoonoses
- Recognize how physicians can apply knowledge of the relationship between planetary health and human infectious diseases to their clinical practice through case studies.
Effects of Climate on Infectious Diseases
Defining Zoonosis
A zoonosis is an infectious disease, which has been transmitted from non-human animals to humans. Zoonotic pathogens can spread through direct contact between the animal and human or indirectly through water, food or other parts of the environment. (2)
The World Health Organization estimates that zoonoses account for one billion cases of illness and one million deaths annually worldwide (1). Studies have found that 58% of all infectious diseases are aggravated by climate change (3). There are numerous events related to climate change that lead to these impacts; warming, precipitation, floods, drought, storms, land cover change, ocean climate change, fires, heatwaves, and sea level have all been found to influence changes in infectious disease patterns (3). The varied pathways through which these events modify disease trends will be described further in this section.
Increased Exposure to Pathogens
Changes in climate resulting in warming and precipitation can bring pathogens in closer and more prolonged contact with humans (3). For example, in the case of vector-borne diseases such as those transmitted by mosquitos, ticks, and fleas, warmer temperatures across broader areas lead to an expanded range where they are able to survive and spread (3). In the US between 2004 and 2018 the number of illnesses from mosquito, tick, and flea bites more than doubled (4).
Climate changes can lead to changes in the geographic distribution of pathogens in other ways as well. Drought can cause mosquitoes and birds to concentrate over the remaining water bodies, increasing transmission of West Nile virus (3). Temperatures in the Arctic are rising at more than twice the speed of the rest of the world and anecdotal evidence of the impact on zoonoses is increasing. An outbreak of anthrax in the Arctic Circle was believed to have originated from an unearthed animal corps following a reduction in frost. Reductions in snow cover have caused voles to find shelter in human inhabitations, leading to outbreaks of Hantavirus and Alaskapox (3, 4).
Changes in human activity related to climate hazards may also increase exposure to pathogens. For instance, heatwaves lead to increased recreational water activity and have been associated with cases of waterborne illnesses such as Vibrio-associated infections and primary amoebic meningoencephalitis (3). Human migration is anticipated to substantially increase in coming decades due in part to climate change (5). This is expected to influence infectious diseases through several pathways including the introduction and spread of infections, as well as the exposure of migrants to endemic diseases to which they do not have immunity (5).
Differences in Pathogen and Host Strength
Climate change has the potential to lead to a number of factors that increase the survival ability of pathogens. For example, warmer climates can increase the transmission efficiency of the West Nile virus by increasing mosquito reproduction, biting rates, and viral replication. Heat also upregulates gene expression of proteins affecting transmission, penetration, and host injury by Vibrio spp bacteria, which cause diarrheal illnesses . Warming and precipitation can also increase the food resources of rodent populations that have been associated with infectious diseases such as plague and hantavirus (3).
Susceptibility to Infections
Climatic hazards can negatively impact the ability of humans to withstand pathogens. Malnutrition – resulting from a number of consequences of climate change including poor crops and damaged infrastructure – can negatively impact human immunity (3).
The impacts of air pollution related to climate change on humans’ susceptibility to infectious diseases are also important to note. Climate change exacerbates air pollution through a number of routes including longer fire seasons, more airborne dust, and increased chemical rates in the atmosphere that influence ozone and fine particulate matter (PM2.5) formation (8). Exposure to PM2.5, NO2, carbon monoxide, and ozone have been linked in children to increased emergency room visits for respiratory infections (8). In adults, exposure to PM2.5 and NO2 has been linked to respiratory infections including increased incidence and severity of pneumonia, increased reporting of upper respiratory tract infections; chronic exposure has been associated with increased COVID-19 incidence and mortality, as well as tuberculosis transmission and progression (8).
Impacts on Human Health
Emerging Infectious diseases (EID)
WHO defines an emerging infectious disease, or EID, as an infectious disease that has appeared in a population for the first time, or that may have existed previously but is rapidly increasing in incidence or geographic range. Many EIDs are zoonoses or start off as zoonoses before spreading within the human population (9).
There is increasing awareness of emerging infectious diseases, such as HIV/AIDS in the 1980s or SARS and COVID-19 more recently. The emergence of novel human infectious diseases is the result of both changes in the geographic distribution of pathogens as well as genetic adaptations in the microorganisms, both of which can be direct or indirect consequences of climate and environmental change. Changes to ecosystems and to migration patterns can also result in infectious diseases spreading further around the globe and create favorable conditions for the re-emergence of previously controlled pathogens Vector-borne infectious diseases are particularly affected, as exemplified by the spread of West Nile virus and Lyme disease in North America and the re-appearance of dengue outbreaks in southern Europe. This combination of factors leads to three expected impacts on infectious diseases in Canada, as summarized in Figure 1. First, there is an increased risk of introduction and endemic transmission of infectious diseases from around the world. Second, a south-to-north spread of some diseases currently endemic to the United States is anticipated. Finally, the re-emergence of Canada-endemic infectious diseases are expected (11).
Vector-borne infectious diseases
Vector-borne infectious diseases are those where the infectious pathogen is transmitted from one person or animal to another via the bite of an arthropod, such as a mosquito or tick.
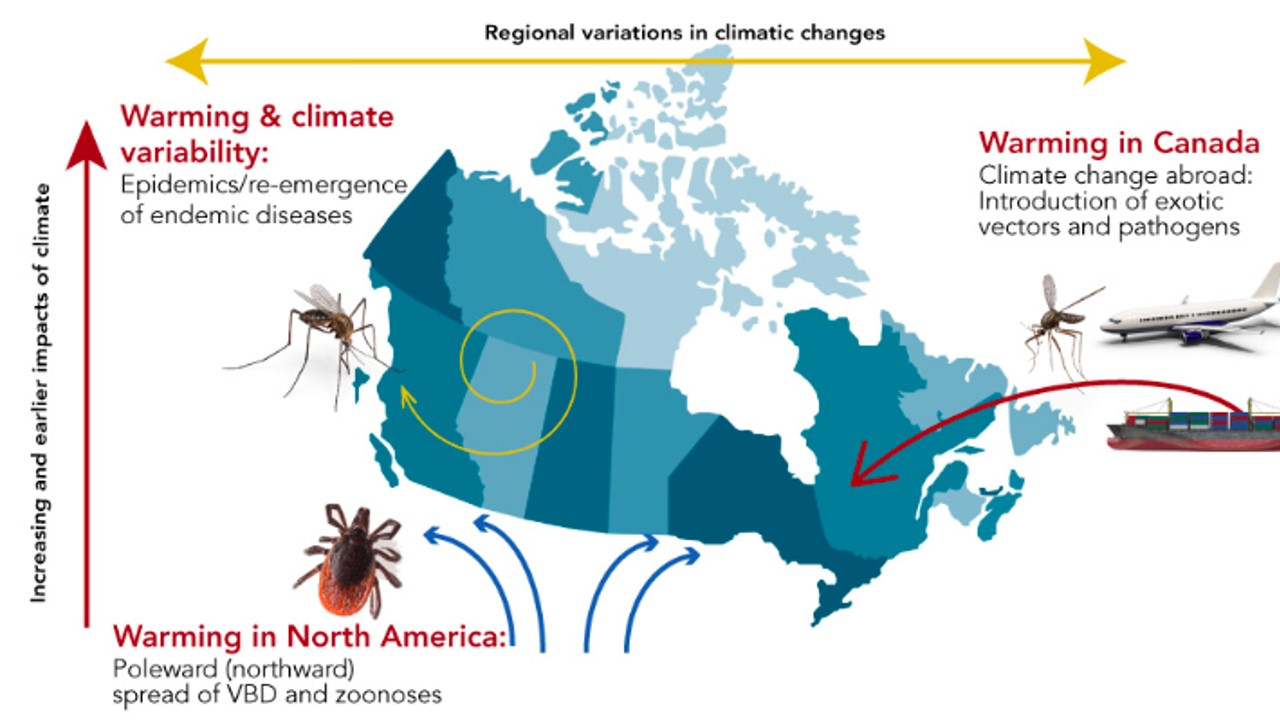
Figure 1. Impacts of climate change on infectious diseases in Canada (11).
Integration Into Clinical Practice
To provide appropriate and timely patient care, physicians must be aware of how climate change is altering infectious disease epidemiology and adjust their differential diagnoses accordingly. For example, tick-borne illness has doubled from 2004 and 2016 with a corresponding geographic spread due in part to warmer temperatures that change habitat suitability for ticks. Lyme disease makes up 80% of these tick-borne illnesses (13). An anticipated lengthened tick season also means that infectious are expected to occur earlier in the spring and linger later into the fall (13, 14). Physicians working in areas without substantial rates of Lyme disease must continue to be vigilant for patients presenting with potentially associated symptoms to avoid a missed diagnosis.
Case Study – West Nile Virus
West Nile Virus provides a useful example to illustrate the impacts of climate change at various stages of infectious disease transmission.
West Nile Virus is caused by a Flaviviridae virus. Although most people infected with WNV remain asymptomatic, it can cause a rash and feverish illness. In a minority of cases, illness will develop further into serious neurological symptoms, paralysis or death. There are currently no vaccines and prevention against infection is based on protective behaviour and barrier clothing.
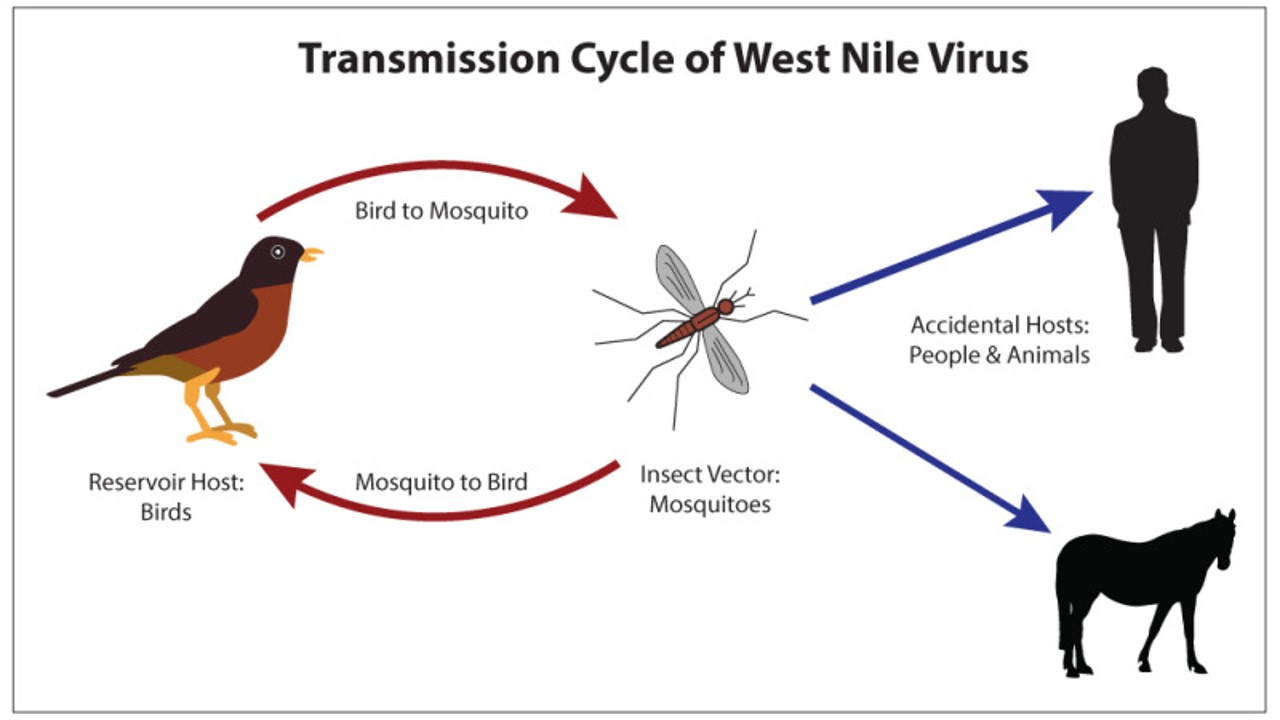
Figure 2. Source: Transmission Cycle of West Nile Virus. Contributed Illustration by Bryan Parker. From: West Nile Virus © 2022, StatPearls Publishing LLC.
Birds are the reservoir host for West Nile Virus, meaning that they provide the site for the virus to live, grow, and multiply. Humans and pets (horses, dogs) are accidental hosts for the virus, meaning that they can be infected and develop disease, but are not part of the natural life cycle of the virus. The disease is vector-borne. Mosquitoes, which are the vector in this case, pick up the virus as they feed on infected birds and then spread it by biting other birds, people or animals.

Birds: Birds are the reservoir of West Nile Virus (15). Warmer than average winters and longer frost-free seasons can impact migration, breeding, and mortality of birds (10, 16). Additionally, droughts and water scarcity have been shown to bring birds and mosquitoes into closer proximity, increasing the cycling of the virus between them (16).
 Mosquitoes: Mosquitoes are the insect vector for West Nile Virus (10). Warmer temperatures will increase the geographic spread where mosquitoes are able to survive and breed. Additionally, while the West Nile Virus transmission season in Canada is typically May through September, warming is expected to increase the period where mosquitoes are able to survive. The transmission season can therefore be anticipated to start earlier and continue later into the fall. In the setting of drought, standing water can increase mosquito populations (15).
Mosquitoes: Mosquitoes are the insect vector for West Nile Virus (10). Warmer temperatures will increase the geographic spread where mosquitoes are able to survive and breed. Additionally, while the West Nile Virus transmission season in Canada is typically May through September, warming is expected to increase the period where mosquitoes are able to survive. The transmission season can therefore be anticipated to start earlier and continue later into the fall. In the setting of drought, standing water can increase mosquito populations (15).
 Humans: Humans are incidental hosts for West Nile Virus. Climate change is expected to lead to human behaviours that bring them into closer proximity with mosquitoes that carry West Nile Virus (10). Physicians must be prepared to manage this increased risk. Assessments must include detailed travel histories, and a broad infectious disease differential should be maintained. Testing capacity of hospitals should be reviewed. Patients must be advised on precautionary measures such as wearing long pants and avoiding early-morning and late-evening exposure to vector insects (16).
Humans: Humans are incidental hosts for West Nile Virus. Climate change is expected to lead to human behaviours that bring them into closer proximity with mosquitoes that carry West Nile Virus (10). Physicians must be prepared to manage this increased risk. Assessments must include detailed travel histories, and a broad infectious disease differential should be maintained. Testing capacity of hospitals should be reviewed. Patients must be advised on precautionary measures such as wearing long pants and avoiding early-morning and late-evening exposure to vector insects (16).
Conclusion
Climate change is expected to contribute to changes in infectious disease patterns including the emergence of new diseases and those appearing in areas where they had previously not been found. It is critical for physicians to be aware of these trends when caring for patients to avoid missed diagnoses and other poor outcomes.
References

